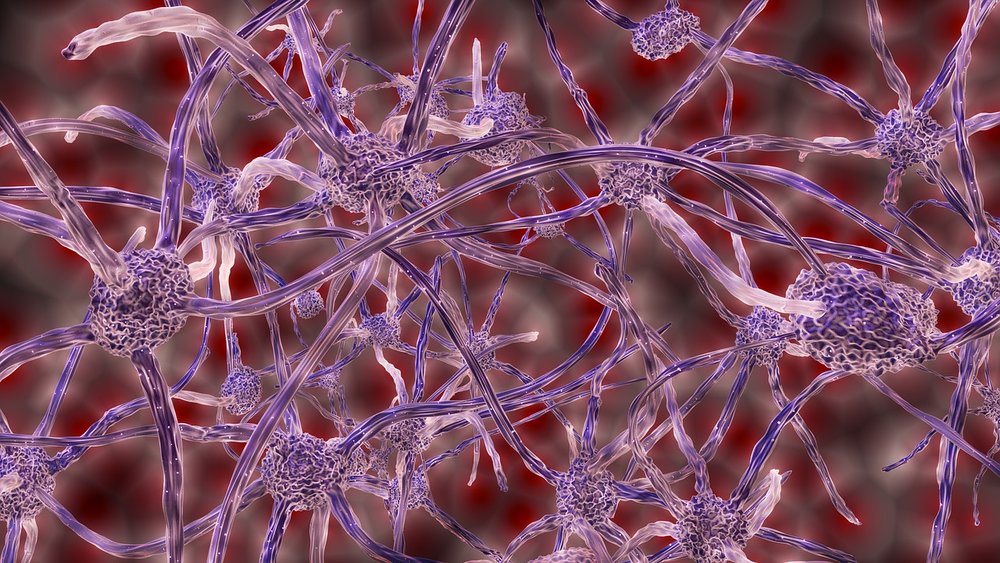
Researchers from Arizona State University and the Icahn School of Medicine at Mount Sinai Indiana University made a large-scale analysis and used data from three different brain banks. They concluded that human herpes viruses are more abundant in the brains of Alzheimer’s patients and may play a role in regulatory genetic networks believed to be behind the onset of the disease. New possibilities for Alzheimer’s treatment, such as antiviral and immune therapy, are now open.
Alzheimer’s disease is the most common form of dementia. The condition was treated merely symptomatically to date, with just a few attempts made in treating it systematically. The idea that viruses might play a role in Alzheimer’s disease exists for some time but it has never been proven. Now, new findings published in the journal Neuron, could give rise to a virus or virus-related biomarkers for Alzheimer’s, and new pathways to target. The researchers took data from “brain banks” of donor tissue, including whole-exome DNA sequencing and RNA sequencing of 622 brains with the clinical and neuropathological features of Alzheimer’s disease, and 322 healthy brains.
“We didn’t set out to find what we found. Not even close. We were trying to find drugs that could be repurposed to treat Alzheimer’s patients, but the patterns that emerged from our data-driven analysis all pointed towards these viral biology themes,” said senior author Joel Dudley, Ph.D., director of the Institute for Next Generation Healthcare at Mount Sinai, in a statement.
Researchers made a “multi-omic” analysis which means they took data from genes, proteins, fats, and other tissue components that were all assessed and represented qualitatively and quantitatively in a complex mathematical model. Clinical assessments of the patients before they passed were used to present their cognitive decline, while tests performed post-mortem provided information on amyloid plaques and tau tangles, physical symptoms of Alzheimer’s disease.
The research group found that brains of those diagnosed post-mortem with Alzheimer’s disease had high levels of the human herpes viruses (HHV), HHV-6a and HHV-7. Normal brains had lower levels of the two viruses. Additionally, they found that herpes viruses played a role in the regulation of amyloid precursor proteins, specifically on amyloid plaques. Their findings support the pathogen hypothesis which says, amyloid beta builds up in the brain as part of the immune response against infections.
“Our work identified specific biological networks that offer new testable hypotheses regarding the role of microbial defense and innate immune function in the pathophysiology of Alzheimer’s,” said Dudley.
HHV-6a is known to decrease levels of a regulator of the innate and adaptive immune systems called miR155. In mice studies, increased deposition of amyloid plaques and behavioral changes were connected with depleting miR155.
“If it becomes evident that specific viral species directly contribute to an individual’s risk of developing Alzheimer’s or their rate of progression once diagnosed, then this would offer a new conceptual framework for understanding the emergence and evolution of Alzheimer’s at individual, as well as population, levels,” said Dudley.
The whole field of Alzheimer’s has relied on beta-amyloid and tau proteins as targets. New hypotheses and angle of approach are needed in order to achieve greater progress. No new therapies emerged in more than 15 years and Alzheimer’s research had many prospects that had shown early promise but crashed and burned in later clinical trial phases.
The researchers admit that the study leaves many unanswered questions: “The results don’t change anything that we know about the risk and susceptibility of Alzheimer’s disease or our ability to treat it today,” said co-senior author Sam Gandy, a professor of neurology and psychiatry at Mount Sinai.
However, they all agree and believe their findings justify further investigation into the pathogen hypothesis of Alzheimer’s.
“I don’t think we can answer whether herpes viruses are a primary cause of Alzheimer’s disease. But what’s clear is that they’re perturbing and participating in networks that directly underlie Alzheimer’s pathophysiology,” Dudley said.
Learn more about the connection between Alzheimer’s disease and herpes simplex virus in the video below:
By Andreja Gregoric, MSc